"What exactly is a Medicaid (or Medicare) Outlier?" I am sure this question is surging through your minds right about know.
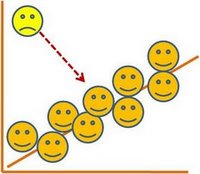
Well, an outlier is something that does not fall within the range of the norm, or beyond the threshold of the amount a hospital gets to cover cases, where cases mean sick people.
According to this report:
In 2003, CMS modified relevant Medicare regulations after reporting that from Federal fiscal years (FY) 1998 to 2002, it paid approximately $9.0 billion more in outlier payments than intended because the outlier calculation overestimated costs for hospitals that increased their charges faster than actual costs.
If you think that $9 billion in excessive Medicare outlier payments is alot, consider the fact that the audit was done for 1998 to 2002, long before IT as we know it today. What do you think the numbers look like for 2003 until know. You do the math.
This occurred because the eight State agencies (1) used outdated cost-to-charge ratios to convert charges to estimated costs and (2) did not reconcile Medicaid outlier payments upon cost report settlement.
No. This occurred because the State Medicaid Fraud Control Units do nothing.
Go ahead and deregulate. Go ahead and lump soothsayer appropriations for Medicare and Medicaid and watch the creation of highly sophisticated revenue-maximization schemes pop up where it will take another decade to find out that Medicaid [and Medicare] Black Grants are breeding grounds for fraud.
No comments:
Post a Comment