 It should be duly noted that there was no mention of Medicaid fraud due to the moritoria on the rules. Medicaid fraud in child welfare is even more perverse as it is excluded from external audits and reviews under the guise of being "in the best interests of children".
It should be duly noted that there was no mention of Medicaid fraud due to the moritoria on the rules. Medicaid fraud in child welfare is even more perverse as it is excluded from external audits and reviews under the guise of being "in the best interests of children". Medicaid fraud in child welfare, particularly Targeted Case Management runs to the tune of hundreds of billions of dollars a year within the Administration on Children and Families.
States Medicaid Fraud Control Units have neglected child welfare fraud since they were created. Until there are contractual debarment, sanctions and more citizen reporting to prosecute and recover from these fraudfeasors, nothing is going to change.
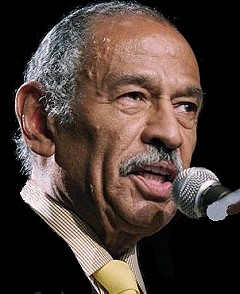
Congressman John Conyers is currently investigating expansions in the False Claims Act, FOIA and Antitrust Law to address this the lack of health care fraud enforcement and I can only pray other leaders join him to preserve the legacy of the nation's most precious treasures, children.
Trileptal was being "illegally and wrongfully" marketed and prescribed to children for off-brand uses such as bi-polar, depression and ADHD, according to the Department of Justice and being billed to Medicaid.
$2.5 billion recovered in health care fraud cases
WASHINGTON - Federal agents recovered $2.5 billion from health care fraud judgments in the budget year that ended in September, a record-breaking amount they credit to whistle-blowers and a renewed effort from the Obama administration.
Health and Human Services Secretary Kathleen Sebelius plans to announce today the money won in cases under the False Claims Act, as well as ways last year's health care law will prevent fraud in 2011. Overall the government recovered $4 billion, including $1.5 billion in administrative findings, rather than court action.
"Our aggressive pursuit of health care fraud has resulted in the largest recovery of taxpayer dollars in the history of the Justice Department," Thomass Perrilli, associate attorney general, said in a statement to USA TODAY. Whistle-blowers received about $300 million in 2010 - from 15% to 25% of the amount recovered - after turning in fraud they saw in the workplace, the government said.
The health care law created on agency and expanded another to help recover stolen money.
The actuary for Medicare expects the provisions of the law to save an additional $4.9 billion in fraud and abuse during the next 10 years. That money will be folded back into Medicare to help it remain solvent until at least 2027.
In 2011, the screening process for new Medicare providers and suppliers will be more strenuous.
More than 19,000 businesses apply every month, but rules will prevent those that have a history of defrauding Medicare or state governments from providing services.
More than half the money recovered came from pharmaceutical companies.
Novartis Pharmaceuticals, for example, agreed to pay $420 million after its owners pleaded guilty to the illegal marketing Trileptal, a medication approved for epilepsy as a psychiatric and pain medicaitno.
Individuals also faced prosecution, including Dr. Todd Scarborough of Melbourn, FLA., who agreed to pay $12 million to settle claims that he improperly billed Medicare for radiation services.
HHS OIG Corporate Integrity Agreement with Novartis Pharmaceuticals Corporation

No comments:
Post a Comment